Millions of endodontic procedures are performed each year and outcome studies have shown that, in over 95% of cases, successful healing will take place. However, there are times when an endodontically treated tooth may exhibit post-treatment disease requiring further intervention.
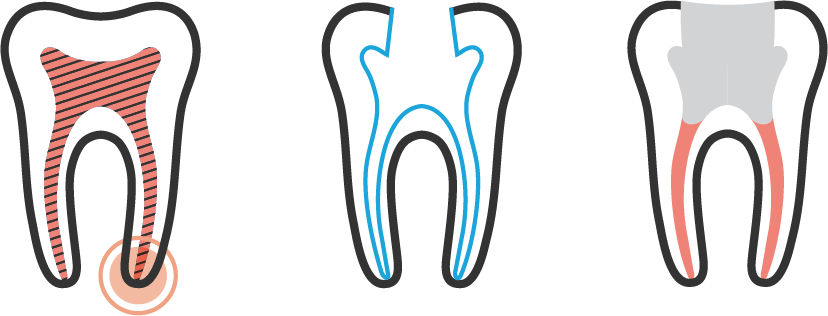
Root Canal Retreatment (Left) Infection or inflammation, after previous root canal treatment, may lead to an abscess. (Center) Previous root canal filling is removed, canals are shaped. (Right) Root canals are resealed. The opening is sealed with a temporary filling.
What is the most common cause of post-treatment endodontic disease?
The most common etiology of post-treatment endodontic disease stems from microorganisms that are retained or reintroduced into the canal system or periapical tissues. This can occur when there is leakage of the coronal restoration, incomplete removal of the infected pulp tissue, iatrogenic complications, apical leakage, or tooth fracture.
Should nonsurgical retreatment be considered?
Prior to undertaking retreatment, it is important to decide if retention of the tooth is in the patient’s best interest. Considerations should include its restorability, periodontal status, significance in the patient’s comprehensive treatment plan, health history, motivation, and desires of the patient. Other treatment options for a tooth that has post-treatment disease include surgical treatment, extraction, or no treatment. Deferring treatment may result in the progression of disease and continued destruction of supporting tissues as well as the potential for acute exacerbations culminating in pain and/or swelling. In most cases, this option would be unacceptable.
Case Highlight
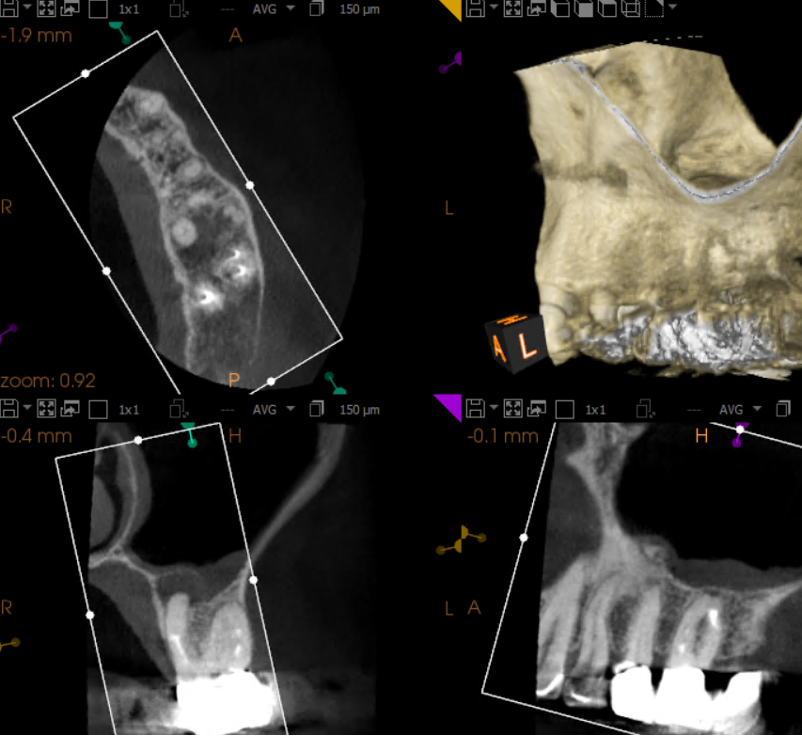
Tooth #14: Maxillary first molar with incomplete root canal and separated instrument


Diagnosis
Patient presented with the chief complaint of a “toothache” that was clinically tender to percussion and localized to tooth #14. Radiographic examination showed an untreated mesiobuccal root and a large post in the palatal canal with no root canal filling evident beyond the post. In addition, there was a separated instrument in the apical third of the distobuccal root. Cone beam CT demonstrated a periapical radiolucency associated with the palatal root. These findings supported a diagnosis of failed endodontic treatment with symptomatic apical periodontitis.
Treatment
Both mesiobuccal canals were located and the separated instrument in the distobuccal root was bypassed so that the canal could be instrumented to the apical terminus. The post in the palatal root was removed and the canal was negotiated. GentleWave® irrigation was performed to enhance canal disinfection. The completion radiograph displays the complex anatomy with significant apical canal curvatures.
